When Wisdom Teeth Meet Trauma: New Clues on Managing Jaw Fractures
A study from Wuhan University reveals that not all wisdom teeth in jaw fractures should be removed — and that personalized treatment could reduce nerve injury risks.
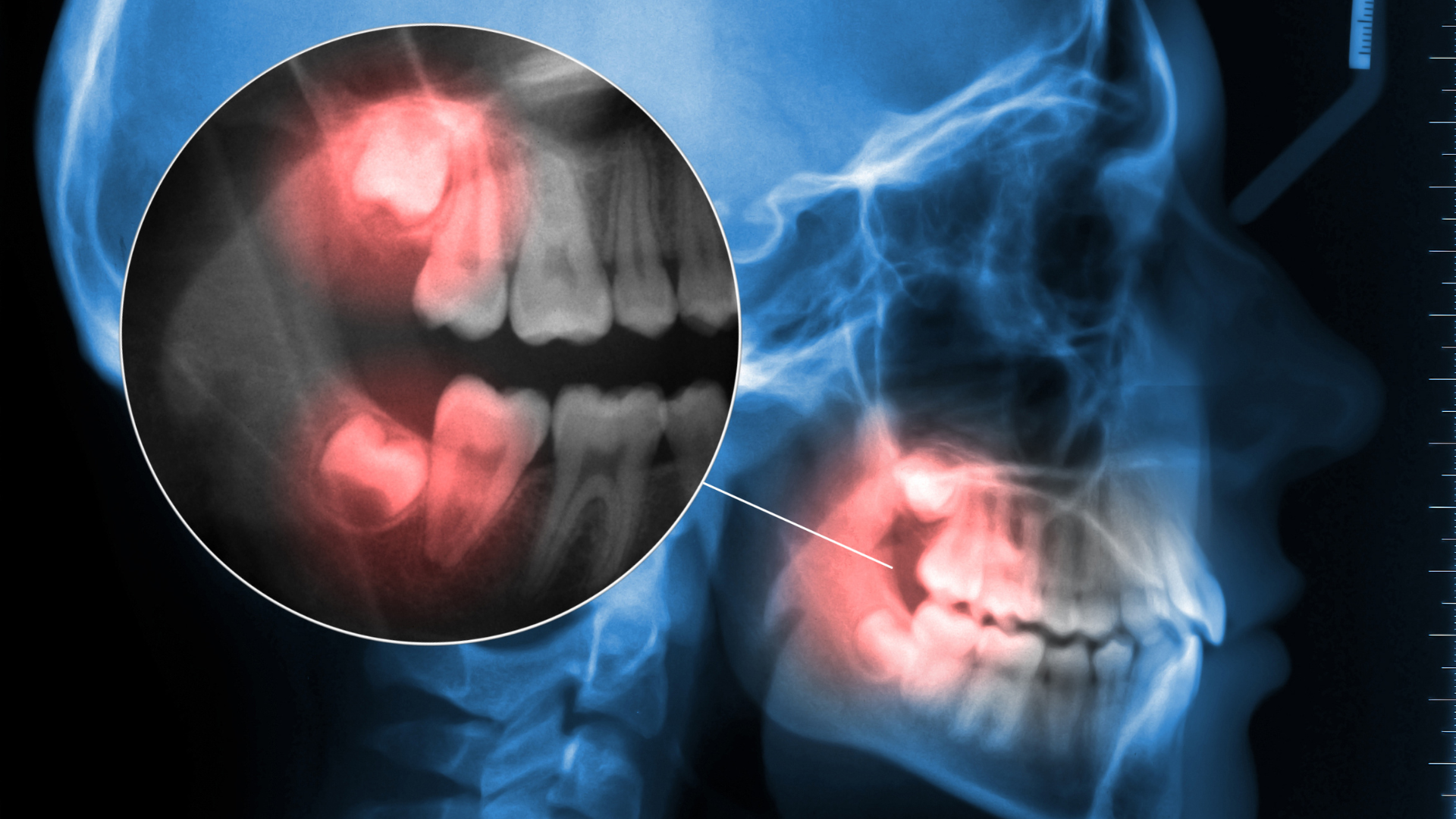
The Overlooked Victim in Jaw Fractures
When the jaw breaks near the back corner — known as a mandibular angle fracture — doctors often focus on repairing the bone. But another structure is almost always caught in the damage: the third molar, or wisdom tooth.
Traditionally, surgeons have debated whether to remove or keep the tooth during surgery. Some believe removal prevents infection; others worry it could cause further trauma or nerve injury. Surprisingly, few studies have examined how the tooth itself is injured during the fracture — until now.
Classifying the Damage: Three Types of Tooth Trauma
Researchers at Wuhan University reviewed 110 cases of patients treated for mandibular angle fractures between 2014 and 2023. Each case involved a wisdom tooth located directly along the fracture line.
They categorized tooth injuries into three new types:
Type I – Complete dislocation: the tooth is forced out of its socket.
Type II – Tooth fracture: the crown or root is broken.
Type III – Stable exposure: the tooth lies along the fracture line but remains intact and unmoved.
Only about 12% of teeth were severely damaged (Types I or II). The vast majority (88%) were Type III — meaning they were affected but structurally sound.
A Tailored Surgical Approach
Based on this classification, the team proposed a “stratified trauma-specific management” strategy:
Remove the tooth if it’s dislocated or broken (Type I or II).
Keep the tooth in place if it’s stable (Type III).
This targeted method aims to balance safety and recovery — avoiding unnecessary extractions that might damage nearby structures, especially the inferior alveolar nerve (IAN), which controls lower lip and chin sensation.
What the Results Showed
The outcomes were striking:
Patients who kept their wisdom teeth had no higher risk of infection or bite problems.
However, those who had teeth removed were more likely to experience nerve injury — occurring in about 10.6% of all cases, but significantly higher in the extraction group.
This suggests that unnecessary extraction might do more harm than good, especially when the tooth remains stable and uninfected.
Why It Matters
The study offers a practical guide for oral surgeons, turning a long-standing gray area into a more evidence-based decision. By classifying tooth injuries and tailoring treatment accordingly, surgeons can:
Reduce nerve-related complications
Shorten surgical time
Preserve natural bone and tooth structure
It also emphasizes that wisdom teeth are not passive bystanders in jaw fractures — their condition can directly affect recovery.
What’s Next
While the results are promising, the authors note that the study’s retrospective nature and modest sample size mean further prospective research is needed. Larger, multi-center trials could confirm whether this approach should become a new standard in oral and maxillofacial surgery.
Reference
Deng, Y.-F., Dong, Q.-Q., Zhao, H.-K., Diarra, D., & Li, Z. (2025). Traumatic characteristics and trauma-specific management of the third molars involved in mandibular angle fractures. BMC Oral Health, 25, 1742. https://doi.org/10.1186/s12903-025-07136-2