The Hidden Cost of Tooth Decay: Why the Poor Pay More
A Global Oral Health Crisis
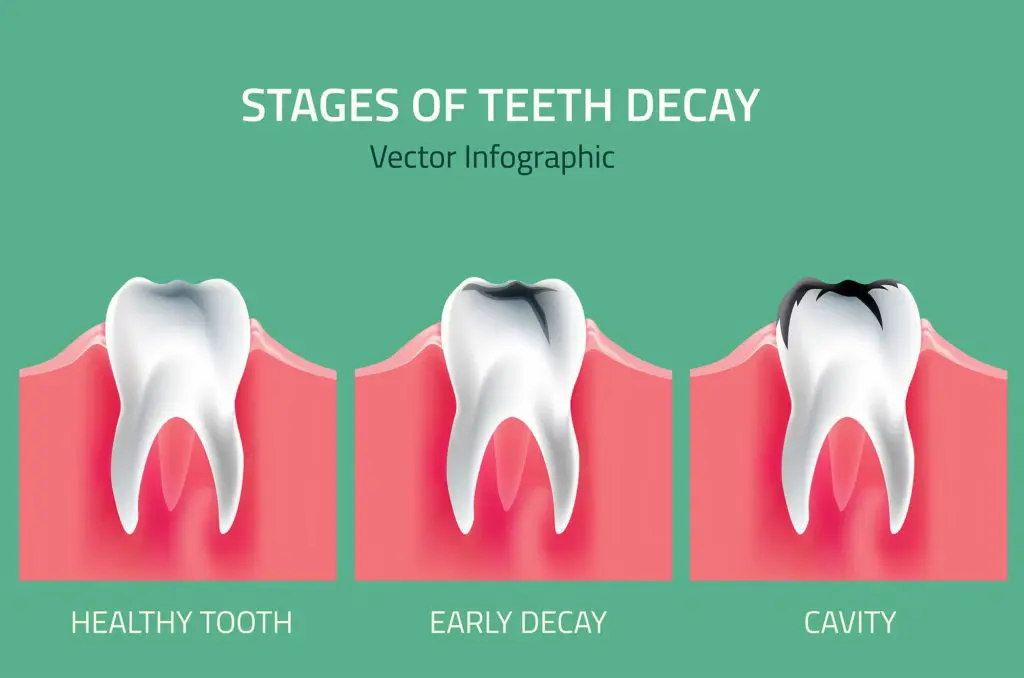
Tooth decay, or dental caries, might seem like a small health issue compared to heart disease or diabetes. Yet according to the World Health Organization, it is the most common non-communicable disease worldwide—affecting an estimated 2 billion people.
Behind each cavity lies a broader story of inequality. A new study published in BMC Public Health by Gerard Dunleavy and colleagues (2024) finds that the economic burden of tooth decay falls hardest on the most disadvantaged communities. Despite being largely preventable, dental caries remain a persistent—and expensive—problem.
Following Six Nations’ Smiles
The study explored the lifetime economic costs of managing tooth decay from ages 12 to 65 across six countries: Brazil, France, Germany, Indonesia, Italy, and the UK.
Using national oral health data and a “cohort simulation model,” researchers estimated how much each country spends directly on treating caries—through fillings, extractions, root canals, and implants—across different income groups.
The findings were striking.
Brazil bore the highest total cost: US$36.2 billion, followed by Indonesia at US$26.2 billion.
On a per-person basis, the UK topped the chart at US$22,910, while Indonesia had the lowest at US$7,414.
In most countries, the poorest groups spent the most—not because they received better care, but because they started with worse oral health and higher rates of decay.
Inequality in Every Tooth
In wealthier and poorer nations alike, tooth decay mirrors social inequality. The most deprived populations tend to have:
Higher sugar consumption, due to cheap processed foods;
Less access to fluoride and dental care;
Limited preventive education.
Even in countries with public dental services, such as the UK, people from deprived areas were more likely to lose teeth than to receive restorative care.
As the authors note, “the healthcare burden stems from a higher baseline caries experience and greater annual progression rates in the most deprived.”
Can Prevention Level the Playing Field?
The researchers modelled two “what-if” scenarios to test the power of prevention:
Universal prevention everyone benefits equally from better oral hygiene and public health measures (like fluoridated water or sugar taxes).
Levelling-up prevention interventions are targeted more heavily toward deprived groups.
Both approaches reduced costs, but the second had a far greater impact.
If preventive efforts were focused on those most at risk, per-person cost reductions ranged from US$3,948 in Indonesia to US$17,728 in the UK.
That means targeted prevention doesn’t just improve health it saves money, too.
From Drills to Prevention
For decades, dental care has centered on repairing damage—drilling, filling, and extracting—rather than preventing decay in the first place. But this “restorative cycle” is costly and unsustainable.
Simple, evidence-based interventions could change that narrative:
Fluoride toothpaste and varnish protect enamel from early decay.
Silver diamine fluoride (SDF) can halt cavity progression, even in low-resource settings.
Community water fluoridation reduces decay rates by up to 26%.
Sugar taxes and better labelling can reduce sugar intake and cavities across populations.
However, access remains uneven. The most deprived often cannot afford fluoride toothpaste or live in non-fluoridated regions, perpetuating the “cycle of decay.”
A Call for Policy Change
The study underscores that oral health is a social justice issue. Preventive care, when accessible and equitably distributed, can dramatically lower both health disparities and national healthcare costs.
The authors argue that it’s time to shift funding and policy toward preventive, minimally invasive dentistry, especially for children and vulnerable groups.
Such measures could not only reduce the global US$245 billion cost of dental caries but also improve quality of life for millions.
As Dunleavy and colleagues conclude, “Transformative changes in oral healthcare funding models are required to realize the financial benefits of preventive approaches and reduce inequalities across socioeconomic groups.”
Reference
Dunleavy, G., Verma, N., Raghupathy, R., Jain, S., Hofmeister, J., Cook, R., et al. (2024). Inequalities in oral health: estimating the longitudinal economic burden of dental caries by deprivation status in six countries. BMC Public Health, 24:3239.