A Simple Brush Test for Detecting Oral Cancer
Why Early Detection Matters
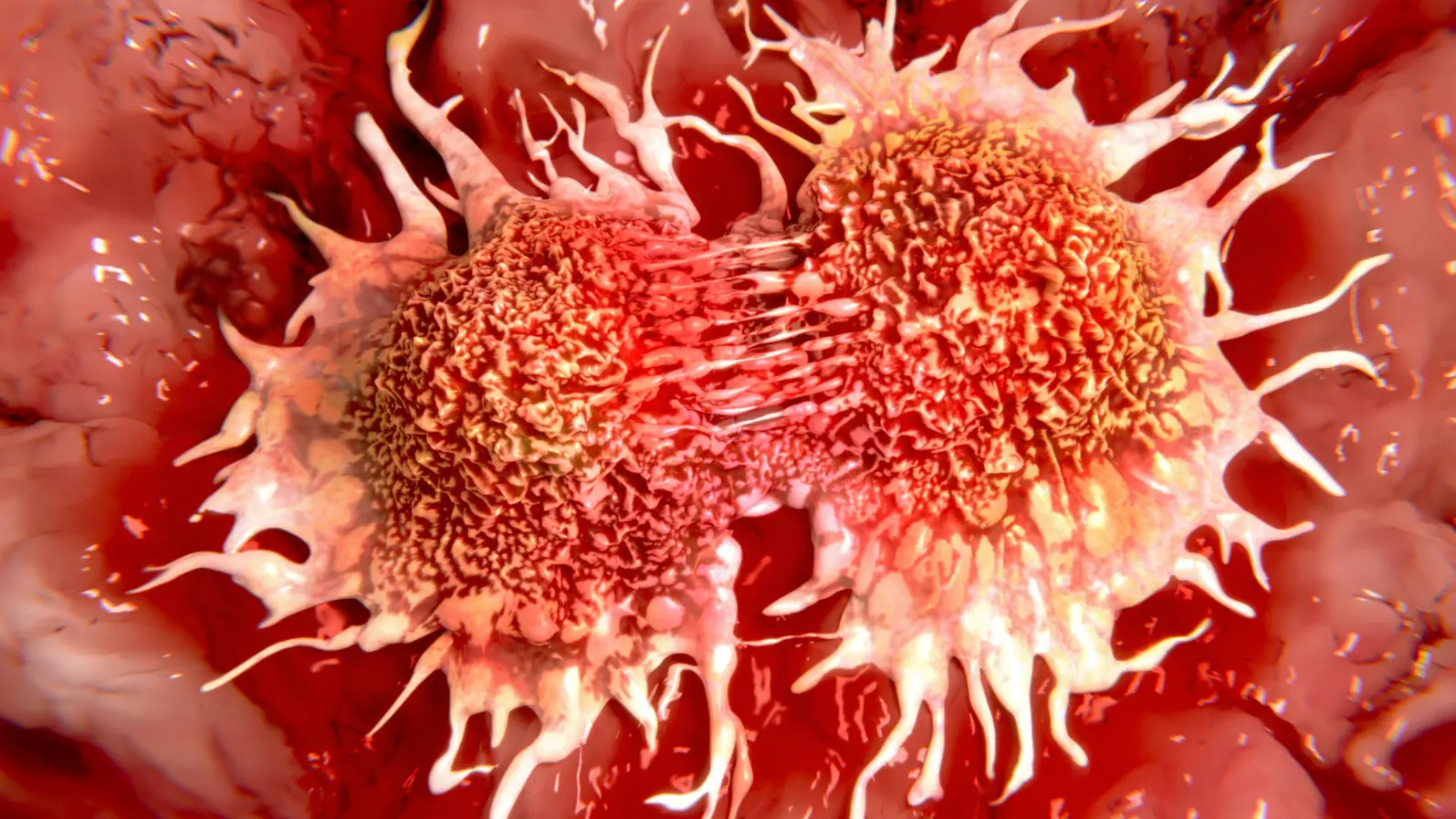
Oral squamous cell carcinoma (OSCC) is one of the most common and deadly head and neck cancers. While it can often be cured if caught at an early stage, many cases are diagnosed too late. Current gold-standard diagnosis relies on biopsies—an invasive, costly, and sometimes stressful procedure for patients. Moreover, repeated biopsies aren’t practical for long-term monitoring of suspicious oral lesions.
This has created an urgent need for a simple, accurate, and non-invasive test that can help clinicians decide when a biopsy is truly necessary.
The Role of Defensins in Cancer
Human beta-defensins are small antimicrobial peptides that help defend the mouth against infection. But in cancer biology, they play a double role. Researchers have found that human beta-defensin 3 (hBD-3) tends to be overexpressed in early oral cancers, while human beta-defensin 2 (hBD-2) is underexpressed. This imbalance suggested a potential diagnostic “signature” that could distinguish malignant from benign oral lesions.
Introducing the Beta-Defensin Index (BDI)
To harness this insight, scientists developed the Beta-Defensin Index (BDI). The test is surprisingly simple:
A soft brush (cytobrush) collects cells from both the suspicious lesion and a normal site in the same patient’s mouth.
The levels of hBD-3 and hBD-2 are measured.
A ratio is calculated, giving the BDI score.
A higher BDI score strongly correlates with the presence of oral cancer.
What the Study Found
In a series of blinded multi-center studies, researchers tested BDI in over 90 patients:
Sensitivity: 98% (ability to correctly identify cancer)
Specificity: 83% (ability to rule out cancer in benign lesions)
These results outperform many existing biomarker-based tests for oral cancer. Importantly, the BDI worked consistently across different clinical sites and examiners, showing its robustness.
Even more exciting, the team demonstrated that the BDI could be adapted into a microfluidic “lab-on-a-chip” device, potentially enabling point-of-care testing right in dental or primary care clinics.
Why It Matters
The BDI test could:
Reduce unnecessary biopsies, sparing patients pain, cost, and stress.
Help dentists and physicians quickly decide when a lesion is high-risk.
Provide a low-cost, non-invasive screening tool—particularly valuable in low-resource settings where pathology services are limited.
Open the door for monitoring precancerous lesions over time without repeated surgery.
The Road Ahead
While promising, the authors note that larger, more diverse international studies are needed to refine cutoff values and ensure consistent results across populations. Future work will also explore whether BDI can be combined with microbial biomarkers for even greater accuracy.
If successful, the BDI could become a powerful tool in the global fight against oral cancer, shifting care from invasive diagnostics toward predictive, preventive, and point-of-care medicine.
Reference:
Ghosh, S. K., Man, Y., Fraiwan, A., et al. (2024). Beta-defensin index: A functional biomarker for oral cancer detection. Cell Reports Medicine, 5, 101447.